What is a "Gap in Care?"
A “gap in care” is defined as the discrepancy between recommended health care best practices and the care that is actually provided.
This can manifest itself in several different ways; the most common include:
- Individuals that are missing age-based or annual screenings or vaccines
- Individuals who do not consult with their doctors over a prescribed medication that might not be appropriate for a patient
- Individuals that are not adding a medication to meet evidence-based guidelines
So, given this definition, how do you identify gaps in care in your population and design benefits programs accordingly? Below are a few key areas to help you get started.
How do you identify gaps in care?
For most organizations, the most challenging part of closing care gaps is identifying care gaps.
Instead of focusing on actionable data that could craft tomorrow’s wellness initiative, too many employers rely on carrier reports that only identify what’s already happened, not what they can do moving forward. This means that organizations are stuck looking in the rearview mirror while trying to drive their healthcare costs down with effective initiatives.
The good news is that forward-thinking benefits leaders and vendors are relying on intelligent solutions to consume all of these disparate data sets and generate actionable insights for their populations.
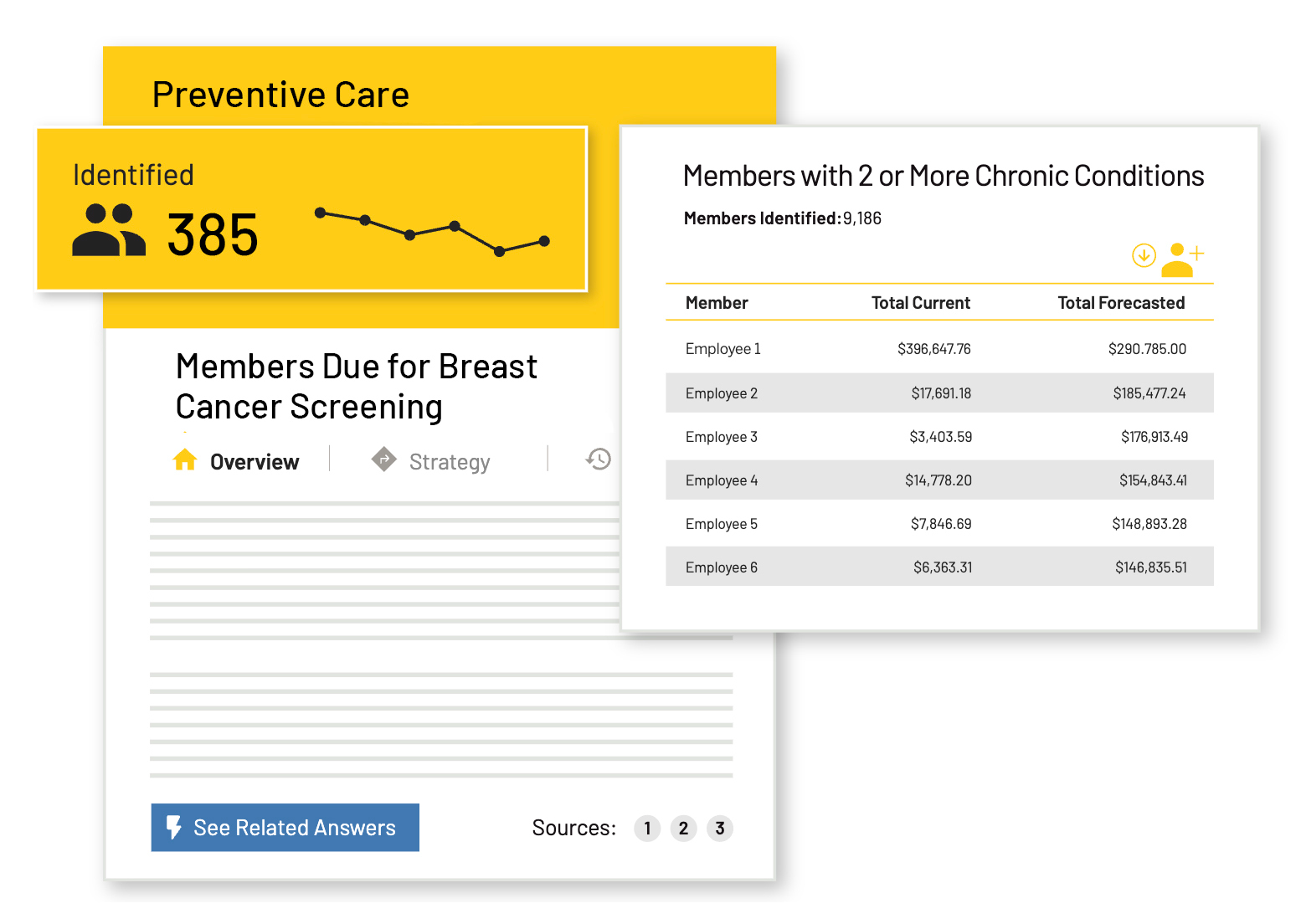
Your healthcare data holds troves of information that can help pinpoint the chronic conditions and unaddressed preventive measures impacting your population. However, data by itself is just that – data. The Springbuk platform pulls all of this data into a single place and takes your analysis a step further by highlighting critical compliance gaps, steps to engage at-risk members, and the savings opportunities if those gaps are addressed.

Want to see 6 ways Springbuk can help you improve the health of your employees? Check out this guide.
Who usually has a gap in care?
Because our Health Intelligence platform monitors gaps in care for thousands of employers across the United States, we have a vast amount of data around the impact that gaps in care have on healthcare spend. While every organization is different, we’ve noticed trends in general healthcare compliance. Based on our research, these are the percentages of members who are compliant to care:
- Diabetes: 3% Member Compliance
- Coronary Artery Disease (CAD): 19% Member Compliance
- High Blood Pressure (HBP): 29% Member Compliance
- Cholesterol: 37% Member Compliance
- Rx Management: 64% Member Compliance
Want to know which care gaps are the most expensive in 2024? Explore our latest Health Trends Report now!

Steps That You Can Use to Close Gaps in Care
Once you’ve identified a gap in care, it is extremely important that you take action. According to the data that we’ve seen from hundreds of employers, organizations could save, on average, $439,000 from members with gaps in care. In fact, 26% of members have a gap in care, but they account for 39% of their total future health spend.
Your next steps will vary depending on the current step-up of your organization’s benefits plans. If you’re interested in identifying and closing gaps of care in your organization, there are a few things that you can do today that can make a giant impact on your future healthcare costs.
Step 1: Get a Grip on Data
The first and most important step you can take is looking at the data that you’re currently collecting on gaps in care. Depending on your broker and analytics provider, you may have extremely robust data around your population gaps. However, you may have nothing but claims data that you have to piece together yourself. These may come in the form of static PDFs and carrier reports, or you may be able to dive into a platform that analyzes the data for you.
Springbuk Insights™, for example, provides detailed information about each member of the population who has a gap in care and projects how much that population will cost you over the next year.
This feature goes beyond analyzing claims and wellness data; it generates actionable strategies and predicts members at-risk of conditions to more effectively guide disease management resources and risk mitigation strategies.
Insights distills your data and curates direction on the next steps you can act on today by:
- Driving immediate impact through the identification of Gaps in Care
- Identifying patterns among your employee population
- Uncovering opportunities to avoid unnecessary procedures, recommend lower-cost drugs, mitigate risk, and improve the efficiency of care
- Targeting populations that are at risk with preventive interventions
- Having a single source of truth between internal stakeholders, vendors, and health solutions.
Step 2: Uncover Actionable Opportunities in Health Data
Once you have a solid understanding of what data your broker and other vendors have provided you, you can use that information to craft your benefits strategy.
For example, after using Springbuk Insights™ to uncover actionable opportunities, employers can turn to Springbuk Activate to answer the question “Who or what can help me manage the opportunities that Springbuk has identified?”
Springbuk Activate matches employers with potential partners based on their population’s health needs, showing them potential opportunities in savings and program engagement – all in one place.
- Activate is entirely data-driven – only the programs that qualify using the employers’ underlying data, such as medical claims or drug claims, are displayed
- A “card” within Activate displays the partner’s logo, program description, value proposition, and strategy for realizing opportunities
.png)
This means that, instead of blindly planning your wellness initiatives activities and educational programming based around intuition, you can design them around actionable data.
Step 3: Evaluate Your Vendors
Finally, after integrating all relevant data points into one system, organizations must analyze their results accurately to make informed decisions on their benefits plans based on up-to-date information about their employees' healthcare needs. Through careful analysis, employers can monitor trends over time in order to uncover opportunities for cost savings or improved engagement levels among employees with their benefits package.
Furthermore, by understanding which services are being used by certain populations or age groups, organizations can curate more tailored strategies when it comes time for open enrollment periods.
Ready to see if your organization is ready to incorporate a solution like Springbuk into your benefits strategy? Check out this guide.









